 Pima County Medical Examiner Greg Hess at his office in Tucson, Ariz. Hess and another Arizona-based medical examiner are rethinking how to catalog and count heat-related deaths, a major step toward understanding the growing impacts of heat.
Pima County Medical Examiner Greg Hess at his office in Tucson, Ariz. Hess and another Arizona-based medical examiner are rethinking how to catalog and count heat-related deaths, a major step toward understanding the growing impacts of heat.
By Alejandra Borunda
Greg Hess deals with death day in, day out.
Hess is the medical examiner for Pima County, Ariz., a region along the United States-Mexico border. His office handles some 3,000 deaths each year — quiet deaths, overdoses, gruesome deaths, tragic ones.
From April through October every year, Hess is confronted with an increasingly obvious and dramatic problem: His morgue drawers fill with people who died sooner than they should have because of Arizona’s suffocating heat.
 Downtown Tucson seen from afar. The skyline of downtown Tucson was ominous during a heat wave last summer. 2023 was one of the hottest years ever recorded in Arizona.
Downtown Tucson seen from afar. The skyline of downtown Tucson was ominous during a heat wave last summer. 2023 was one of the hottest years ever recorded in Arizona.
Pima is hot, but it’s not the hottest county in the country. Nor the biggest; the most humid; or the most populated. But Hess and his team are at the country’s forefront in one key way: They have developed some of the most innovative strategies to accurately count the number of people dying from heat-related problems. Those efforts could redefine how the United States understands the growing cost of climate change, because right now, the human toll of climate-worsened disasters is dramatically undercounted.
A small group of health experts across the country has concluded over time that thousands of Americans die every year because of climate-fueled disasters, like stronger, more dangerous hurricanes or heat waves so intense they obliterate historical records. And no one is keeping official track of the scope of the problem — not government agencies, researchers or state officials.
Those omissions aren’t just painful for the loved ones of the dead, says Kristie Ebi, a public health and climate epidemiologist at the University of Washington. They have concrete consequences: Without an accurate count of the human toll of weather disasters, it is hard — or sometimes impossible — to understand their full impact on families and communities. By extension, Ebi says, an incomplete count impairs the ability to plan for and prevent such losses in the future, like knowing when and where to locate cooling centers during a heat wave.
“If you don’t know how many people suffer and die in disasters, then you can’t set priorities appropriately,” she says.
But now a small contingent is trying to count better — a critical goal as climate change pushes heat to nearly unlivable temperatures, makes hurricanes deadlier and chokes communities with wildfire smoke. The ranks are diverse, from those on the front lines of death, like Hess, to epidemiologists and public health experts. And their goal is to provide insights based on their data so that policymakers, city leaders and advocates have the information needed to save lives.
A heat-curious medical examiner
Hale, ruddy-cheeked Hess grew up in Wisconsin, but he has thrived in the desert. He rides his bike to and from work, even through the blazing Arizona summer heat, and he is the undisputed champion of the office’s ongoing pickleball competition (evidence: a small silvery cup on his office shelf, a pickleball jammed inside and a stamped label reading “CHAMPION”).
When he was in medical school, he rotated through a forensic pathology stint, which other students avoided. After all, wasn’t being a doctor about saving people, they asked? What was the point of working on someone who was already dead? But that was part of the appeal for Hess. There was a mystery in these people on the autopsy table, entire lives encapsulated in the bodies that remained.
Plus, upon first meeting, his new department head asked Hess about his beer preferences. This was the place for him, he thought: on a team of people who were, despite their deeply serious work, playful, thoughtful and creative.
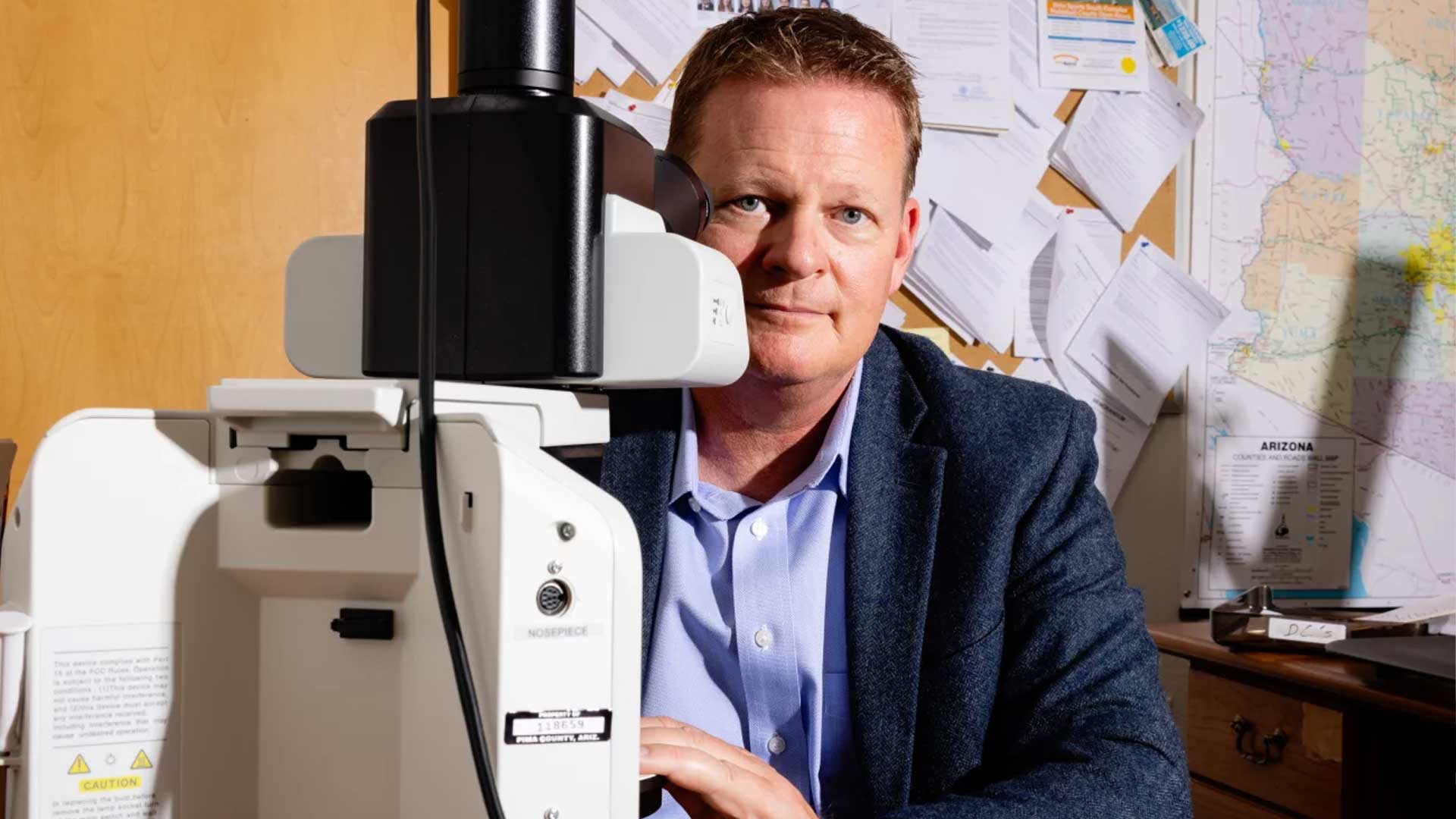 Greg Hess is one of a small cohort of medical examiners and coroners seeking to more accurately keep track of disaster-related deaths nationwide.
Greg Hess is one of a small cohort of medical examiners and coroners seeking to more accurately keep track of disaster-related deaths nationwide.
Hess did a residency in Wisconsin and a stint as an Air Force doctor in California. But when he took the lead medical examiner position in Pima County, Ariz., in 2011, he ran headlong into a crisis — one that would inform his work for years to come.
Pima County is tucked up against the U.S.-Mexico border in southern Arizona. It’s a small county — about a million people, most of whom live in Tucson. The rest is rural, swaths of desert crisscrossed by roads stripped pale by the incessant sun. When Hess arrived, the county was a hot spot for people attempting to cross the border on foot from Mexico into the U.S. But the desert was punishing. Every few weeks during summer after summer, Hess got a call asking his death investigators to go to a scene where two, or six, or eight people had been killed by heat and exposure. The annual counts ran into the hundreds.
The nonstop stream of complicated deaths pushed Hess’ team to develop innovative protocols. They learned how to thoroughly investigate each death, identify those lost, and track down family members left behind, to give them some sense of closure. Hess developed a deep appreciation for the data his team produced and what it could do.
A few years later, the opioid epidemic slammed into Pima and filled the office’s autopsy tables. Once again, Hess and his team leaned into their experience collecting thorough, complete data describing and humanizing the deaths. And as always, Hess collated all the data into neat annual reports. But he suspected they sat on someone’s desktop, unread. The reports were packed with valuable insight, but their utility was limited because they were “not very timely,” he said.
But around this time, during the height of the opioid epidemic, other officials — from county public health, the mayor’s office, the police force, the federal government — realized that death data could help prevent more deaths by identifying patterns quickly and figuring out how to intervene. But that would require a faster exchange of data. So in 2022 Hess got the go-ahead to hire an epidemiologist, Tasha Tully, to mine the rich seam of information the team collected. She developed a near-real-time dashboard that tracked opioid deaths and funneled useful insights to the city and state offices.
Before long, Tully and Hess realized such efforts could help them understand another, quieter epidemic: the avalanche of deaths from each hotter and hotter summer.
 VIEW LARGER Hess and his team have years of experience producing and curating thorough, useful data. Public health offices use that data to develop solutions to the problems of the day, from opioid deaths to heat deaths.
VIEW LARGER Hess and his team have years of experience producing and curating thorough, useful data. Public health offices use that data to develop solutions to the problems of the day, from opioid deaths to heat deaths. Why heat?
The biggest, most obvious, directly climate-influenced risk to people’s lives comes from heat.
Climate change has dramatically increased the risk of heat in every state and territory of the United States in recent years. Nationally, summer high temperatures have increased by just under 2 degrees Fahrenheit since the 1970s. But that small number belies the dramatic impact: A small shift in the average temperatures means extremes become much more likely — and much more deadly. Events like the 2021 heat wave that shattered temperature records in the Pacific Northwest would have been virtually impossible absent human-driven climate change, scientists found. So would 2023’s 31-day-long run of 110-plus F temperatures in Phoenix, Ariz.
The Centers for Disease Control and Prevention estimates that each year about 1,200 people in the U.S. die of problems directly caused by heat, such as heatstroke; that number has risen from about 700 just a few years ago. But that’s a vast undercount, says Greg Wellenius, an environmental epidemiologist at Boston University. The true toll, according to a 2020 statistical estimate from Wellenius’ lab, is likely at least 10,000 people every single year.
The discrepancy arises, in part, because the CDC’s estimate is based on whether heat is recorded on someone’s death certificate. But for a host of reasons, heat is rarely listed as a cause of death — even when it plays a major role.
“If somebody doesn't report it, we don't know about it,” says Kathryn Pinneri, a former president of the National Association of Medical Examiners.
Heat is not commonly mentioned on death certificates because heat alone is rarely the main thing that kills people. Typically, hyperthermia deaths are easy to spot, Hess says: What’s trickier to identify, yet much more common, are deaths from other health problems that were exacerbated by heat.
There is no doubt that heat worsens health problems. In hot weather, the number of cardiac arrests rises. The number of strokes goes up. Complications from diabetes increase. Deaths associated with neurodegenerative diseases like Alzheimer’s increase.
 VIEW LARGER The St. Francis Cooling Center offers some temporary relief for Tucson's homeless population from the summer's extreme weather.
VIEW LARGER The St. Francis Cooling Center offers some temporary relief for Tucson's homeless population from the summer's extreme weather. But linking a heart attack to heat is trickier. For that, you need data, collected at the very place where someone died: Was it 120 degrees Fahrenheit inside the home? Was someone working on a roof hours before they collapsed? That specific evidence is what Hess’ office now excels at uncovering.
Hess describes a scenario he’s encountered more times than he can count. His office gets a call about an unhoused person found dead in a park, drug paraphernalia next to them on the ground. At autopsy, the forensic pathologists find drugs in the deceased's bloodstream. In the past, when they filled out their software and death certificate, they almost certainly would have noted it as an overdose death alone, Hess says. But heat makes drug use more dangerous: Methamphetamine inhibits sweating. Opioids like fentanyl inhibit users’ awareness of heat. Cocaine makes people more active.
“We sure do get a lot more of those unhoused people dead in the park with overdoses in July than we do in December,” Hess says. “And so, why? ‘Why’ is because heat may contribute to those deaths.”
So now, when death investigators go out to the body, they’ll note that it was 115 degrees outside. Then, when they fill out their paperwork, they will note the heat — and likely enter it as a contributing factor to the death. That attribution then shows up on the death certificate.
Sometimes the connection between heat and someone’s death is even harder to figure out. What if an older person with a heart problem dies in their home, a trailer that has never had air conditioning, Hess asks? How hot does the room have to be to have been too hot for that person to survive? People who certify deaths are careful: They want real, solid evidence to support their decisions.
If a medical examiner or coroner sees an edge case with no context about heat, “they are going to use their best judgment and say, I don't have enough evidence to make that claim, and therefore I won't make that claim. How would you?” Hess says.
But the evidence does often exist, Hess and other medical examiners say. Creating systems to collect and analyze that evidence is what their offices do differently than many others. The evidence is not as stark as a ligature mark, or chemical traces in someone’s blood, but contextual clues instead. It’s up to the medical examiner, coroners and the death investigators who go to the scene to collect them.
Clue hunters
Hess knew that another medical examiner had already spent several years thinking deeply about the accuracy of death tolls: Jeff Johnston, the energetic forensic pathologist who had stepped into the lead role in Arizona’s Maricopa County in 2013.
Maricopa enfolds Phoenix, the poster child for heat risk. Phoenix’s summer temperatures regularly hover well above 100 degrees Fahrenheit for weeks. Nearly 40% of the city is paved, trapping daytime heat in concrete and asphalt and keeping overnight temperatures stifling. Doctors, houseless advocates, government officials and residents have recognized for some time that the conditions in Phoenix have made it a deadly place to live.
 Heat-related illnesses during the Southern Arizona summers can be dangerous and even deadly. Salvation Army Cooling Centers or “Heat Refuges” are open to all, and provide a climate-controlled space to eat, relax, and re-hydrate.
Heat-related illnesses during the Southern Arizona summers can be dangerous and even deadly. Salvation Army Cooling Centers or “Heat Refuges” are open to all, and provide a climate-controlled space to eat, relax, and re-hydrate.
The problem was, no one really knew exactly how deadly. Like Pima, Maricopa based its estimates on the number of death certificates that mentioned “heat” as the primary cause of death or as a major contributing cause.
But in 2018, Johnston told the 16 forensic pathologists on his team to try something new: Think about heat deaths more expansively. They would track not just heat-caused deaths — the obvious cases, like heatstroke — but heat-related deaths as well.
They came up with a protocol. Every time the office gets a call about a body, they send a “death investigator” to suss out the context in which someone died. Between April and October, those investigators ask about heat. They check the temperature of the rooms people were found in. They ask whether they were having trouble paying their electric bill because of air conditioning. They see whether a phalanx of fans was set up in front of the chair in which someone died.
All that context feeds into the decisions pathologists make when examining the body and filling out death records and goes into the official records themselves. They coined the term “environmental heat exposure” to encapsulate heat-related factors that contributed to someone’s death without necessarily being the primary driver.
“There is some art in deciding what's significant or not,” Johnston says. Hard science, yes, but also nuance, and curiosity and creativity in trying to piece together the last fragments of someone’s life. “It’s hot every summer: 103, 105. The question is, what’s too hot?”
In the mid-2010s, Maricopa reported 61 to 182 heat deaths per year. But after they changed their count technique, the numbers swelled: In 2020, there were 323; 339 in 2021; and 645 in 2023. The numbers were alarmingly large. But they were certainly more representative of what had been happening for years — just not recognized.
None of the changes were complicated. But the shift in mindset is revolutionary, says Rebecca Sunenshine, head of Maricopa County’s Public Health Department.
Data from Johnston’s office was used to make the case that utilities shouldn’t shut off people’s power in the summer, even if their bills were overdue. That 2019 policy shift has likely saved lives, says Sunenshine. In Pima, the Public Health Department is exploring ways to use Hess’ data to figure out where to put cooling centers and to identify those at excessive risk from heat, such as people who live in mobile homes.
Tully, the forensic epidemiologist in Pima, sees the data she produces as the foundation for better decisions. “It's the beauty of my job, I think. It’s being able to be like, OK, we're going to put information out that people haven't had before,” she says. “If public health officials don't have those numbers, they can't identify a problem. They can't try to address a problem, and they certainly can't find solutions to a problem they don't know exists.”
The way forward
Johnston and Hess were among the first medical examiners in the country to adopt the new protocol, with a few tweaks that made more sense for his smaller office in Pima County.
Adoption elsewhere has been slow. “We have a fragmented death investigation system right now in this country,” says Kelly Keyes, president-elect at the International Association of Coroners & Medical Examiners. There is no nationally consistent method by which the people involved in death investigations decide whether a death is related to a disaster in the first place, she says. On top of that, Keyes says, “There is no central repository of death information other than the death certificates.” So if crucial information doesn’t make it onto those certificates, there’s little or no hope of retroactively finding that lost context.
This burst into public awareness after 2017’s Hurricane Maria, the storm that devastated Puerto Rico. Initial government counts suggested 64 people died in and after the storm. But Puerto Ricans knew that number was an extreme undercount. Statisticians looked at the number of deaths recorded in the weeks following the storm and compared that to previous years with no storms, a technique to calculate “excess mortality” from an event like a hurricane or a disease wave (the technique was used to estimate COVID-19 deaths, as well). Those estimates put the true number in the thousands. The official record now stands at 2,975, nearly 50 times the original.
Afterward, a congressional bill required the National Academies of Sciences, Engineering, and Medicine to assess the disaster-death counting capabilities in the U.S. The ensuing report explains that “there are no standard practices” for deciding whether deaths are disaster-related, and it identified “persistent, systemic” flaws in the current system, from inadequate guidance on how to count disaster-related deaths to poor use of the invaluable data that does exist. It recommended systemwide reform of death-assessment efforts nationwide.
But that change has not happened. The CDC last published best-practice guides for how to more expansively account for disaster-related deaths in 2017 and has conducted just a few training sessions for death certifiers since then.
In the meantime, the National Association of Medical Examiners has been pushing its members to adopt standards it recommended in 2022. Johnston presented on Maricopa’s strategies at a late 2023 meeting of medical examiners, and other jurisdictions are considering adopting similar measures. But overall, it is slow going, says Pinneri.
“It really is going to vary amongst the jurisdictions and how the deaths are actually reported to the medical examiners and coroners,” she says. “And that is something we cannot control at all. We can beg and plead and say, ‘You need to report these,’” but the standards are voluntary, and offices are often overstretched, Pinneri says.
The challenges are not unique to heat. Climate change is also raising the risks from hurricanes and wildfires — and death tolls of those events are similarly hard to track.
Wildfire smoke inhalation is rarely, if ever, documented as a primary or even contributing cause of death, though many medical professionals and public health experts think it is driving hundreds, or even thousands, to premature death each year. Similarly, medical examiners, coroners and doctors struggle to attribute many people’s deaths to hurricanes, especially if those deaths aren’t immediate. When a falling tree branch kills someone during the storm, that would be tallied. But what about the case where the storm knocks out the power to someone’s ventilator, asks Keyes? Or someone who couldn’t get dialysis because the clinic flooded? “Where is that on the scale?” she asks.
The omissions are not purely academic. The Federal Emergency Management Agency, or FEMA, provides funds for funeral costs if someone’s death is associated with a federally declared disaster — but it has to be listed on the death certificate. Many who lost family members to Hurricane Maria were denied those funds, absent direct attribution on the certificate. And heat isn’t even considered a “natural disaster” eligible for federal aid.
Other challenges abound. Of the 3,000 different medical examiners, coroners and justice of the peace offices nationwide, only about 50% of them are even using computerized case management systems, Keyes says. And in recent years, the field of death has been “extremely taxed,” she says. The opioid crisis, COVID-19 and ongoing disasters — the relentless crises have stretched thin the few thousand people in this line of work nationwide.
Five years into Johnston’s experiment in Maricopa, there’s just starting to be enough years of data to show that the office’s new protocols are effectively revealing the scope of the heat problem.
 The Arizona desert is punishing. Without adequate water and opportunities to cool down, it can be deadly when temperatures climb.
The Arizona desert is punishing. Without adequate water and opportunities to cool down, it can be deadly when temperatures climb.So far, though, the deaths are only increasing. The 2023 summer broke nearly every heat record in Arizona. The 35-day stretch of 110-plus temperatures pushed the office near a breaking point.
“It's really an emergency response, a crisis response, these last two summers,” Johnston says. In a normal summer, the office handles about 25% more bodies than during the rest of the year. “We're prepared for that. That's our norm,” Johnston says, but “the last two summers, they've been 63% above that.”
Some weeks saw twice as many bodies as usual. His team of 30 was doing 80 scene investigations a week. They rotated shifts so the exam tables in the mortuary were constantly in use, just to keep up with the flood of bodies coming in. Maricopa released the final count of 2023’s heat-related deaths in April of this year: 645.
“It's all a balancing act of trying to respond to what is essentially a mass fatality event,” Johnston says. “It's really hard. The last two summers have been really, really hard.”
In April of this year, just a few days after the 2023 Maricopa death toll was issued, the heat in Arizona was back. The temperatures at Hess and Tully’s midday pickleball competitions cracked 100 in April. The death investigators are packing thermometers in the bags they take to scenes. Hess sent around an email reminding the forensic pathologists to go through a heat-focused checklist in their autopsies. By April, Pima recorded its first heat-related deaths of the season; the teams are bracing for another challenging year.
Hess knows there’s only so much his office can do. But “if you can't articulate what the problem is, then how can you talk about solutions?” Hess asks. “We're not the solution people. We're just the medical examiner's offices, the objective data people. And we just give other people the data and say, here, figure it out.”
By submitting your comments, you hereby give AZPM the right to post your comments and potentially use them in any other form of media operated by this institution.