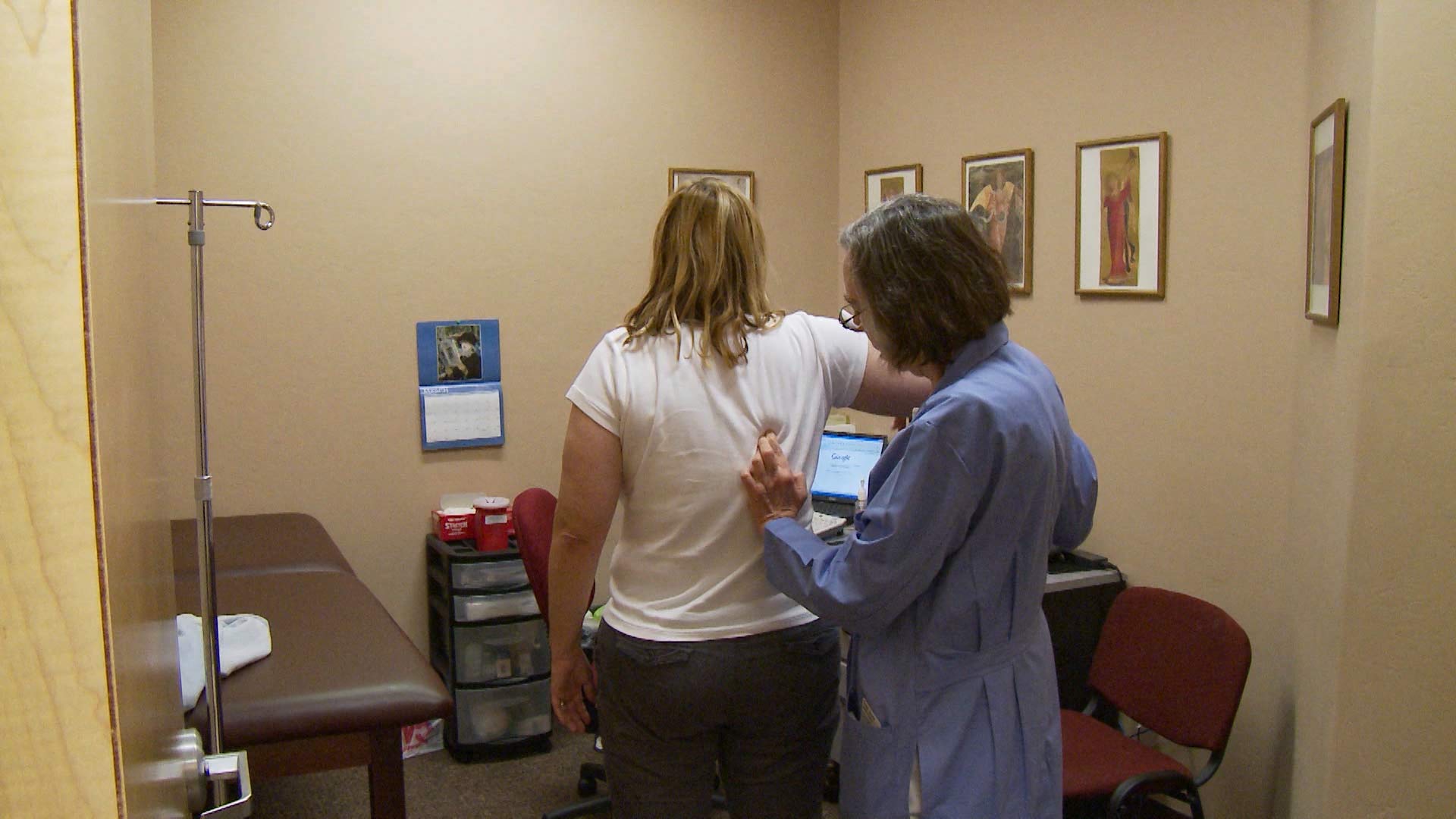
 A health professional examines a patient.
A health professional examines a patient.
For the past six months, the nation has been undergoing a Medicaid “unwinding,” wherein millions of individuals who were enrolled in Medicaid health insurance during the COVID-19 pandemic are being disenrolled because their current income makes them ineligible.
States are now removing people from their enrollment systems because the enhanced federal funding that paid for expanding Medicaid during the COVID-19 pandemic, is ending.
The state agency that handles Medicaid payments to Arizona residents is the Arizona Healthcare Cost Containment System (AHCCCS). On April 1, AHCCCS began the process of running all 2.5 million Arizonans enrolled on Medicaid through federal databases that verified a certain number of people were still eligible to stay on Medicaid automatically.
AHCCCS sent renewal forms to those who were not automatically eligible, to either check their information for errors or verify that they are, in fact, over the income limit.
Heidi Capriotti, communication administrator for AHCCCS, said they have been reevaluating and redetermining the eligibility of enrollees by looking at income and medical criteria, and reaching out to members for additional information if needed.
“As of Sept. 8 of this year, we have initiated renewals for approximately 1.5 million people, and we have about 1 million people left to go,” Capriotti said.
Capriotti said the main cause for disenrollments is people not responding when additional information is needed.
So far, 32% of renewals have been approved and 11% have been discontinued. A third of those who have been disenrolled from Medicaid in Arizona are children.
“People need to respond,” Capriotti said. “We also encourage people to respond even if they think they are no longer eligible. Especially parents because children may be able to move to CHIP, the Children’s Health Insurance Program (KidsCare), even if parents don’t meet Medicaid eligibility criteria.”
In some states, children have been removed from Medicaid coverage because their parents exceeded the adult eligibility limit, even though the children still met the qualifying criteria.
On Aug. 30, the Centers for Medicare & Medicaid Services issued a call to action about these state system issues. According to the agency, “nearly 500,000 children and other individuals who were improperly disenrolled from Medicaid or CHIP will regain their coverage.”
Arizona has been evaluating family members on an individual basis. This means that even if a parent doesn’t meet Medicaid qualifications, their children could still meet the criteria and be transitioned to CHIP.
Matt Jewett, director of health policy for Children’s Action Alliance, said this approach of automatically renewing eligible children even when their parents are ineligible is the right way to do it.
Another call to action came on Sept. 29 from the U.S. Department of Health and Human Services, which sent a letter to state health officials reinforcing that states “must provide 12 months of continuous coverage for children under the age of 19 on Medicaid and the Children’s Health Insurance Program (CHIP) beginning January 1, 2024.”
AHCCCS is increasing the eligibility limit for CHIP on Nov. 1 and as a result, Jewett predicts 12,000 new kids will be enrolled.
Jewett said if people are over the income limit, AHCCCS sends the application to the health insurance marketplace and someone will reach out to the family about alternative health coverage.
“If they go over to the health insurance marketplace, they may pay very expensive copays or have high deductibles,” Jewett said. “So we want to keep them in AHCCCS and get care if possible, but the marketplace is much more affordable than it used to be.”
Claudia Maldonado, director of outreach and enrollment for the nonprofit organization Arizona Alliance for Community Health Centers, said she’s witnessed families who lost Medicaid coverage but found affordable alternatives through the marketplace.
“There’s a lot going on,” Maldonado said. “So just the fact that we have a whole community in this state that is dedicated to helping people go through this renewal process or applying for marketplace health insurance is really critical to make sure that we are keeping people enrolled, and most importantly guiding them through these changes.”
She said her organization’s goal is to keep community members from going without health insurance.
“We are linking arms with our Medicaid program, all the health plans, and the community at large to help as many people as possible,” Maldonado said.
To aid in navigating both the Medicaid system and the healthcare marketplace, the statewide coalition Cover Arizona provides assistance through this website. It matches individuals based on their ZIP codes with organizations that can offer support in-person, by phone, or virtually.
An automated communication service called AHCCCS Connect was launched this year to make it easier for Arizonans to find out more information about their enrollment. People can visit Health-e-Arizona PLUS to sign up for email and text alerts to be notified about their application status if they were approved or denied, their renewal dates, and if any action is needed on their account.
“The ability to text and email people has really helped the responsiveness. I think that’s why we’re seeing, in August, the highest percentage of people remain eligible because they either respond, they’re automatically determined to be eligible, or they’re getting the message and responding to our requests for information,” Capriotti said.
By submitting your comments, you hereby give AZPM the right to post your comments and potentially use them in any other form of media operated by this institution.